Web sample pediatric history and physical exam. History and physical is the most formal and complete assessment of the patient and the problem. Web the documentation template includes the following sections: Date and time of h&p: This is the first admission for this 56 year old woman, who states she was in her usual state of good health until one week prior to admission.
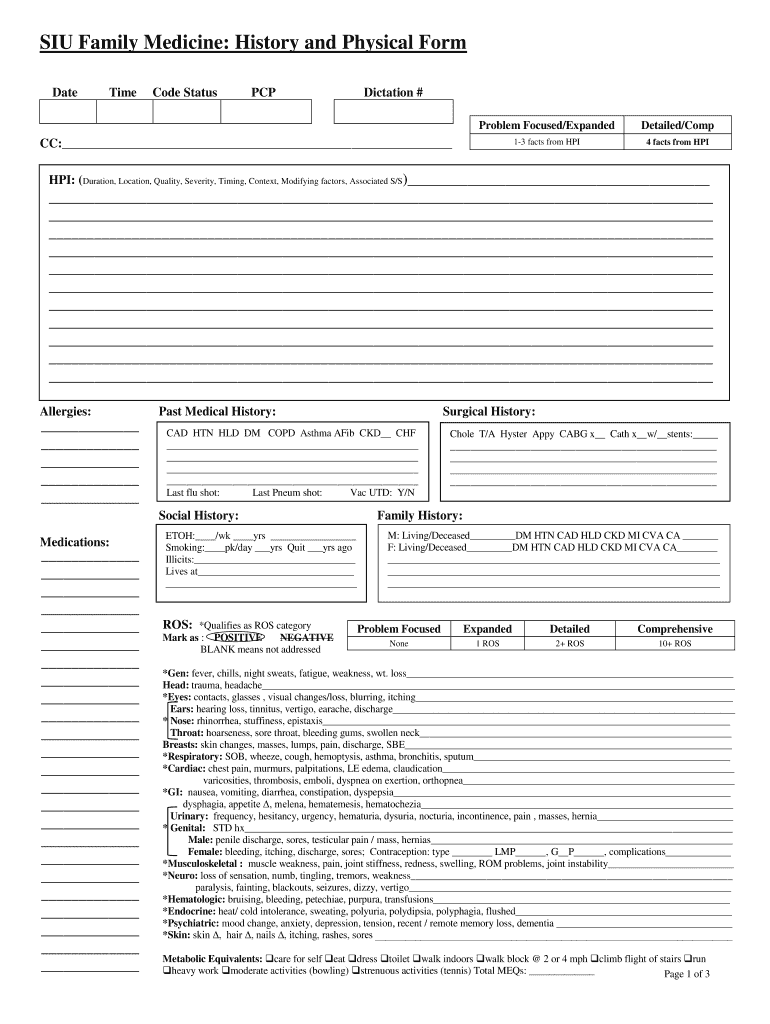
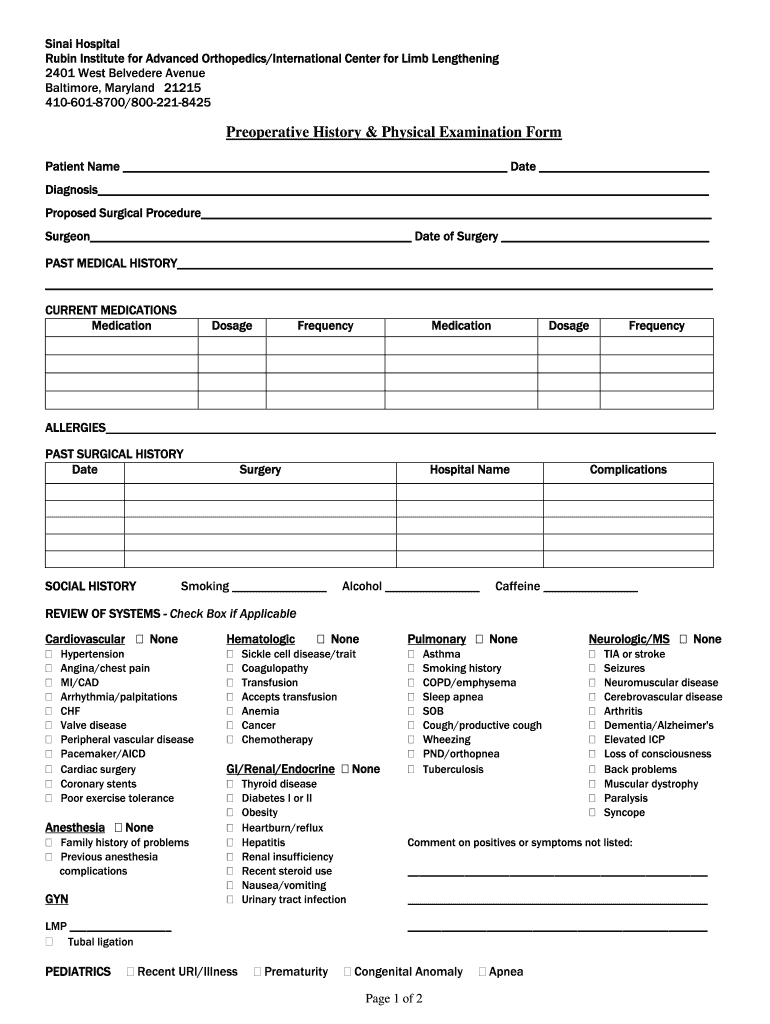
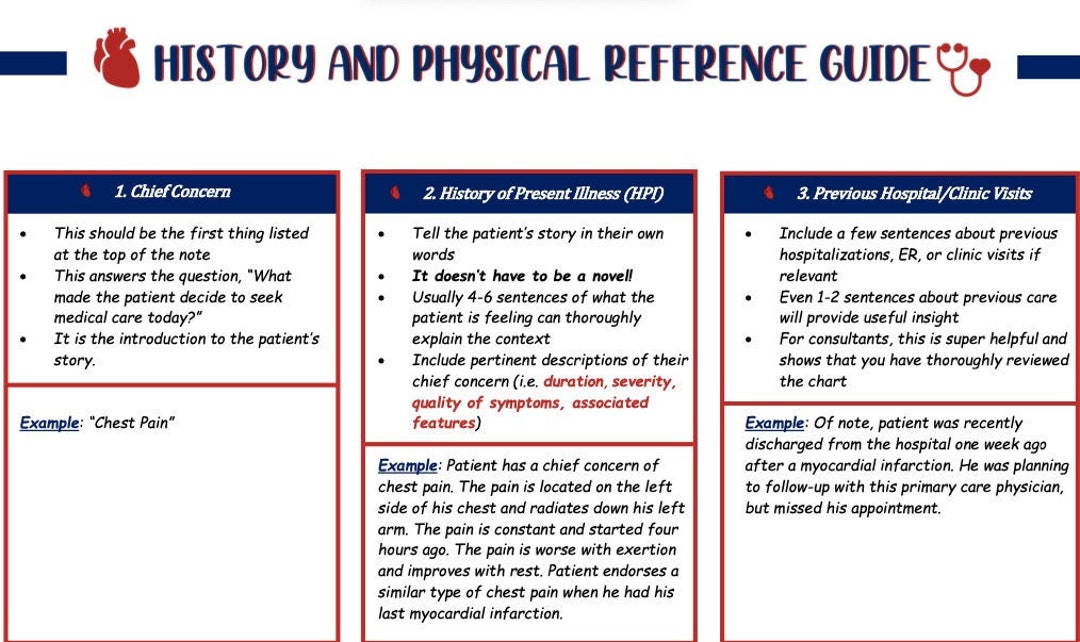
Web as a tool to teach this critical aspect of medicine, students are required to complete and submit to the clerkship office six detailed history and physical examinations. Web history and physical form is a standard medical form that doctors use when they first see a new patient. Web the written history and physical (h&p) serves several purposes: Web history and physical examination (h&p) examples. Web history of present illness:
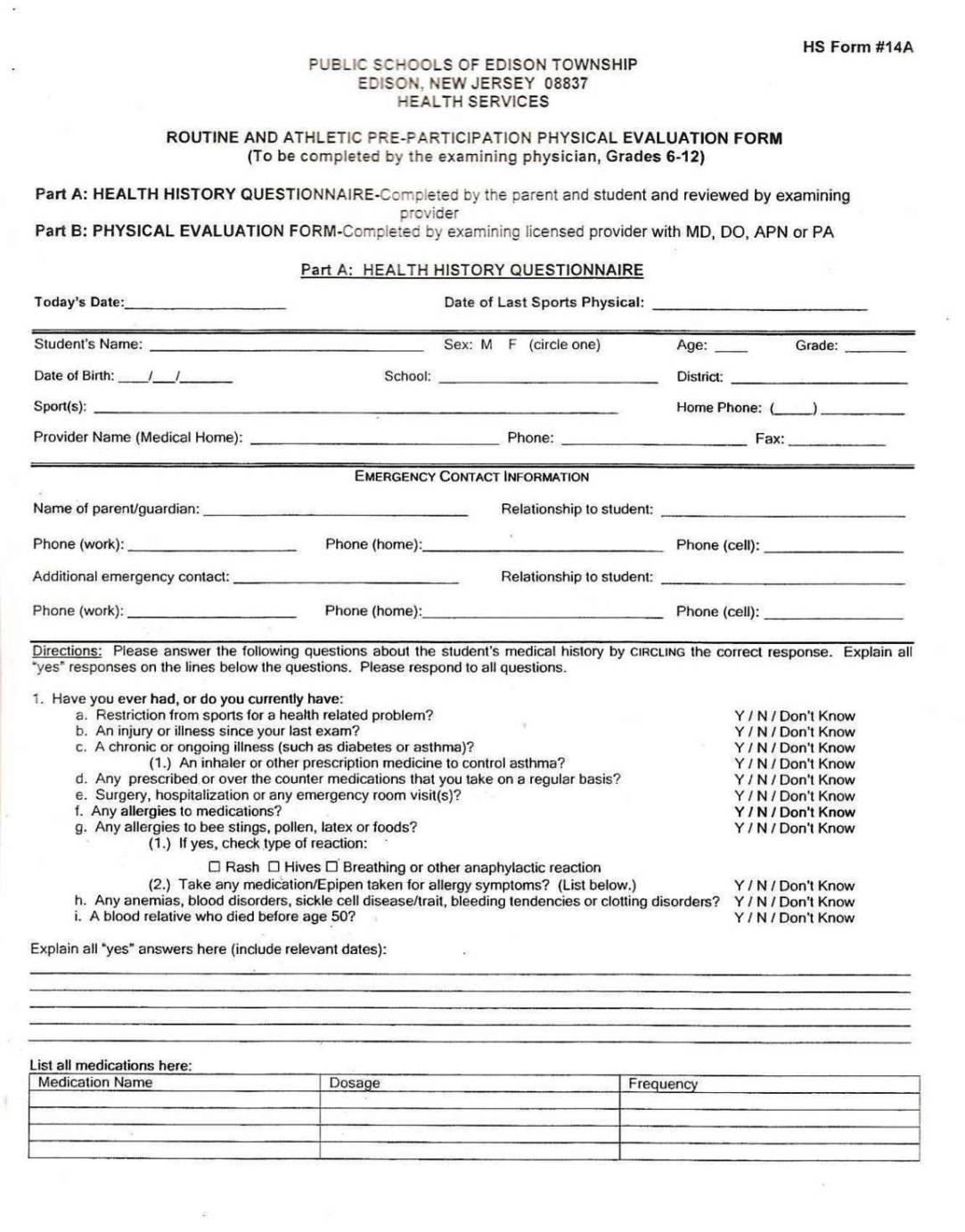
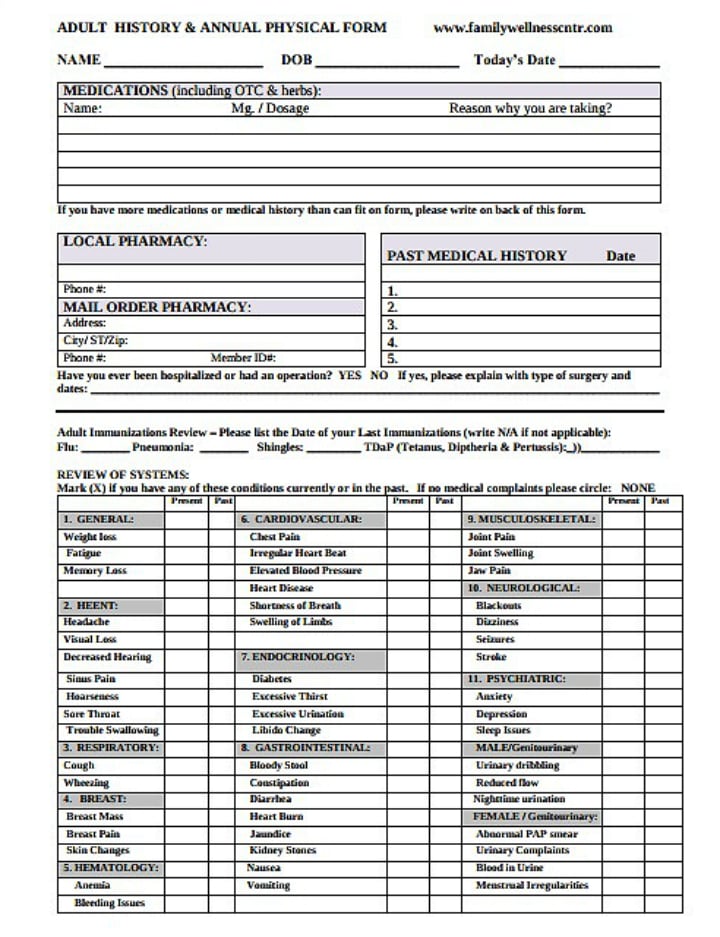
This is a 51 year old gentleman with no significant past medical history presenting with 3 weeks of worsening dyspnea on light exertion, chest pain,. Purpose of written history and physical. Chief complaint (reason for the visit) history of. (please check all conditions that you have or have had) none. Web as a tool to teach this critical aspect of medicine, students are required to complete and submit to the clerkship office six detailed history and physical examinations.
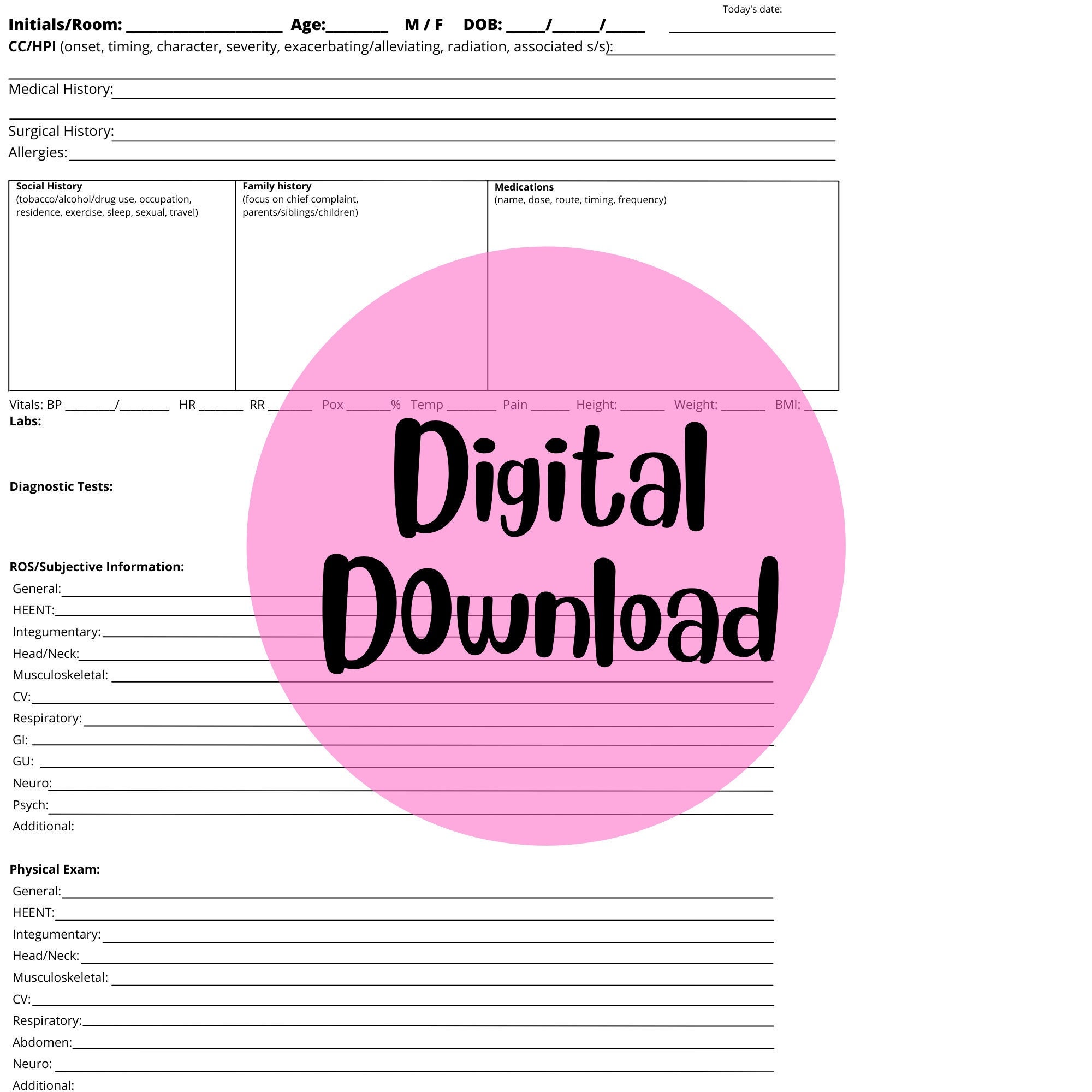
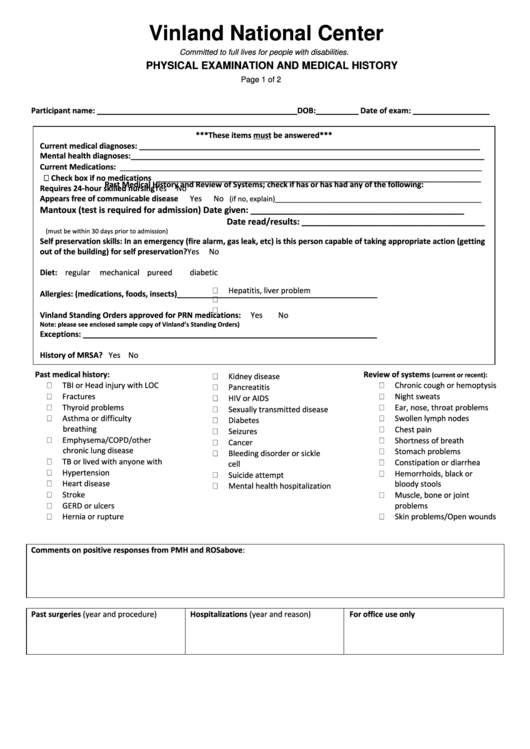
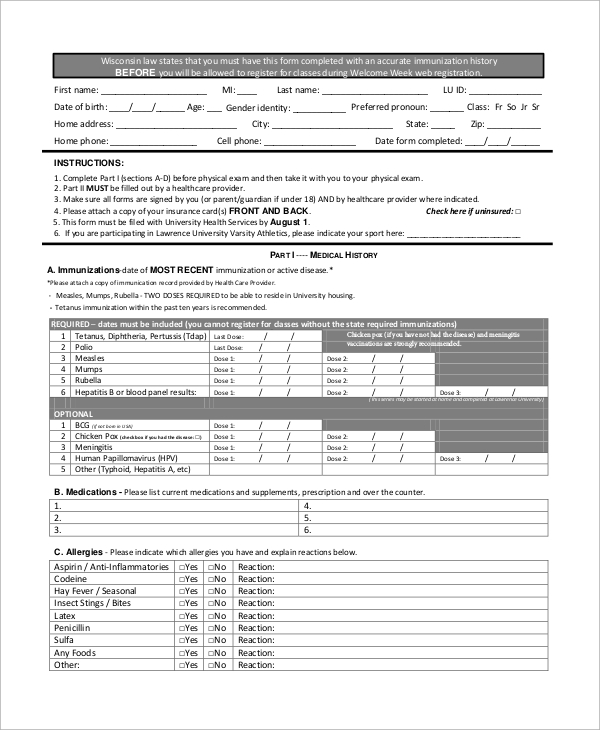
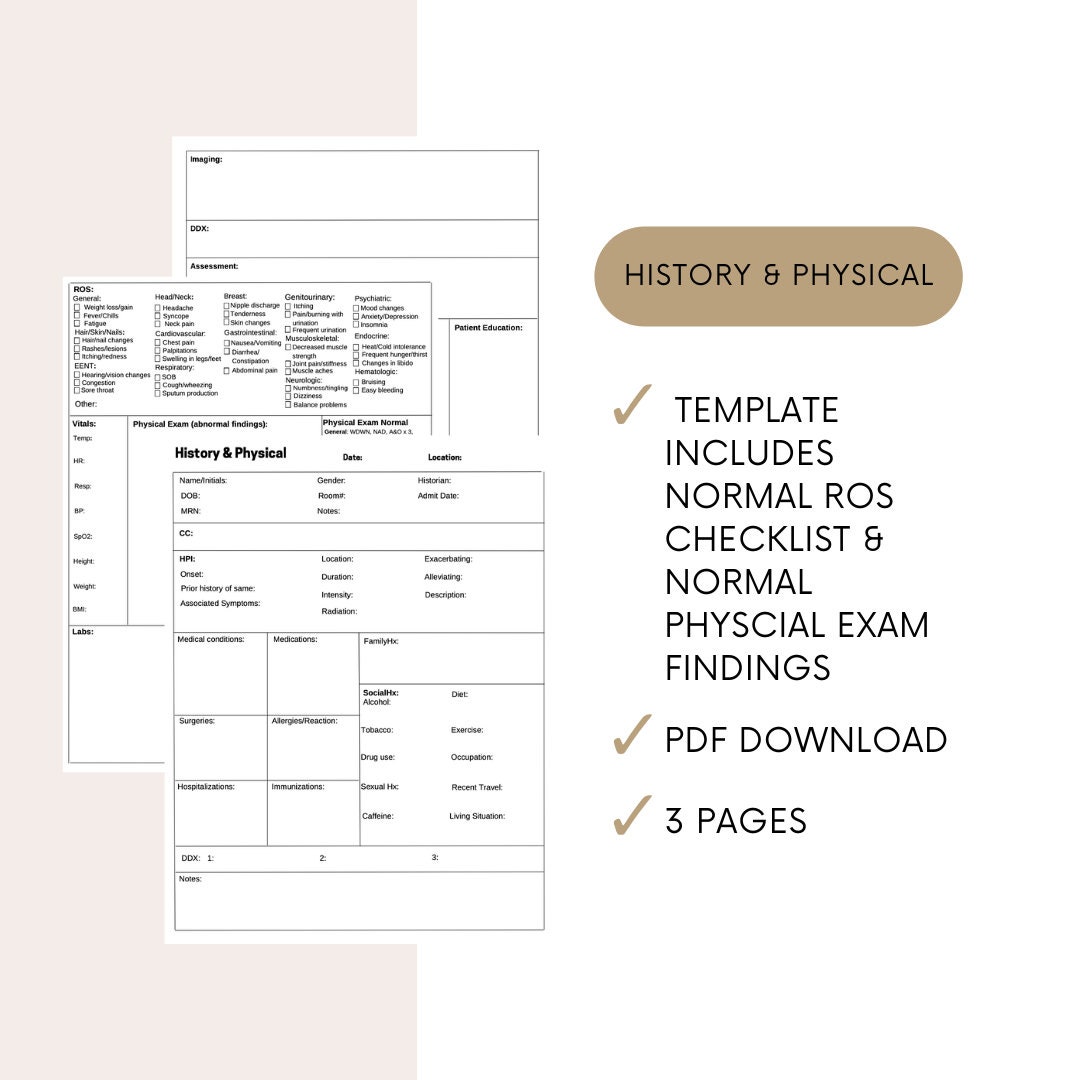
Enter fin (not mrn) state your name, patient name, patient mrn and fin, admitting attending, date. Web history physical documentation of history and physical exam patient name (initials only) dob: The links below are to actual h&ps written by unc students during their inpatient clerkship rotations. Web class i a normal, healthy patient. The surgeon (physician of record) may complete the medical clearance h/p form for the patient, or defer it to the primary. Class ii a patient with mild systemic disease. Web sample pediatric history and physical exam. Web this document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Web the written history and physical (h&p) serves several purposes: Web history and physical examination (h&p) examples. Skin bruising, discoloration, pruritus, birthmarks, moles, ulcers, decubiti, changes in the hair or nails,. Web history of present illness. Purpose of written history and physical. Class iii a patient with severe systemic disease that limits activity but is not incapacitating.
Web History Physical Documentation Of History And Physical Exam Patient Name (Initials Only) Dob:
Web history & physical (short form) date: Web history of present illness: Web as a tool to teach this critical aspect of medicine, students are required to complete and submit to the clerkship office six detailed history and physical examinations. Web the documentation template includes the following sections:
Web A History And Physical Form Is A Foundational Document Healthcare Professionals Use To Gather Comprehensive Information About A Patient's Medical History.
Web history and physical examination (h&p) examples. “i got lightheadedness and felt too weak to walk” source and setting: It is an important reference document that provides concise information about a patient's history and. This is the first admission for this 56 year old woman, who states she was in her usual state of good health until one week prior to admission.
Web These Resources Provided A Detailed Description Of How To Write A Comprehensive History And Physical Examination And A Daily Progress Note.
Web history and physical form is a standard medical form that doctors use when they first see a new patient. Web comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. Web guidelines for history and physical 1.
Web This Document Contains A Patient Intake Form Collecting Demographic Information, Chief Complaint, History Of Present Illness, Review Of Systems, Past Medical History, Social.
Keep in mind that individual styles. Web history of present illness: History and physical is the most formal and complete assessment of the patient and the problem. Web class i a normal, healthy patient.